Coronavirus and Ocular manifestation
Coronavirus and Ocular manifestation
What is Coronavirus?
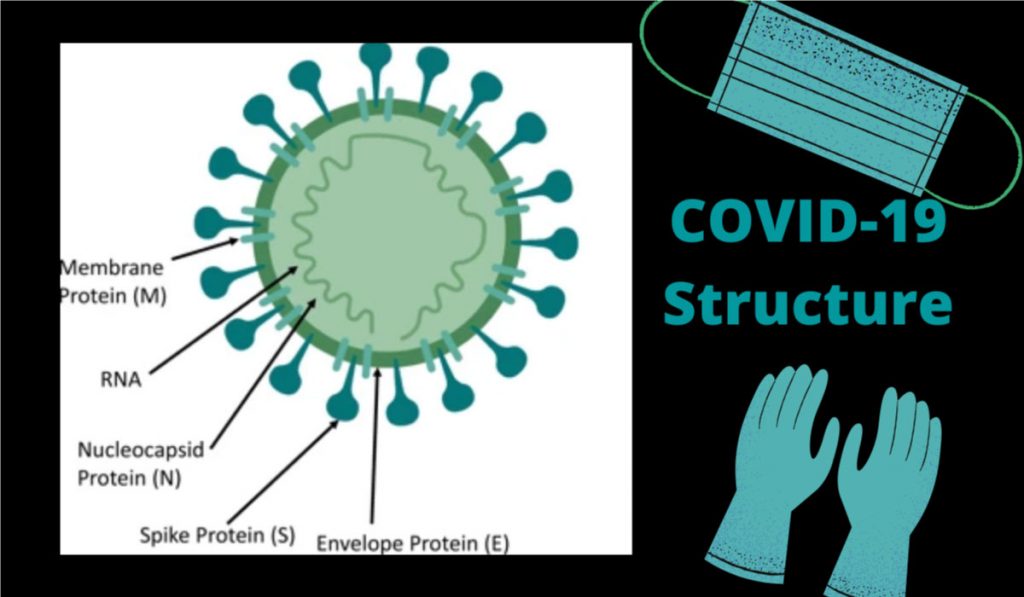
Structural protein
Function of Protein
Nucleocapsid Protien (N)
Bond to RNA genome to make up nucleocapsi
Spike Protein (S)
Critical for binding of host cell receptors to facilitate entry to host cell
Envelope Protein (E)
Interacts with M to form viral envelope
Membrane Protein (M)
Central organizer of CoV assembly & Determine shape of viral envelope
When a virus spread from animal to human its called Zoonotic virus. The official name of this virus is SARS-COV-2. “COVID-19 is the name of the disease it causes, which stands for “Coronavirus disease 2019.” Corona as in crown. The virus is named for its crown-like spikes. It spreads through droplets when we sneeze, cough or speak and can enter the human body directly through eyes, nose or mouth. This virus can also live on a lot of surfaces for hours, so people might pick it up on their hands and this way they can likely infect themselves if they touch their face. The average person who touches its face is approximately 20 times an hour.
Once this virus is inside the body, that spike acts as a key, locking onto the proteins found on the outside of many human cells. Once it has broken in the virus gives the cell instructions to produce more copies of itself. This way the virus starts invading more and more cells in the human body. This manifestation can lead to a fever, cough and fatigue. This further potentially leads to shortness of breath, sore throat, loss of appetite, diarrhoea, loss of sense of smell, lack of taste.
Current Stats of COVID-19 as of 30th August 2020
*Percent change in the number of newly confirmed cases/deaths in past seven days, compared to seven days prior.
Raising questions about Coronavirus and Eye related problems.
But the most important question is - Can COVID-19 transmits through eyes?
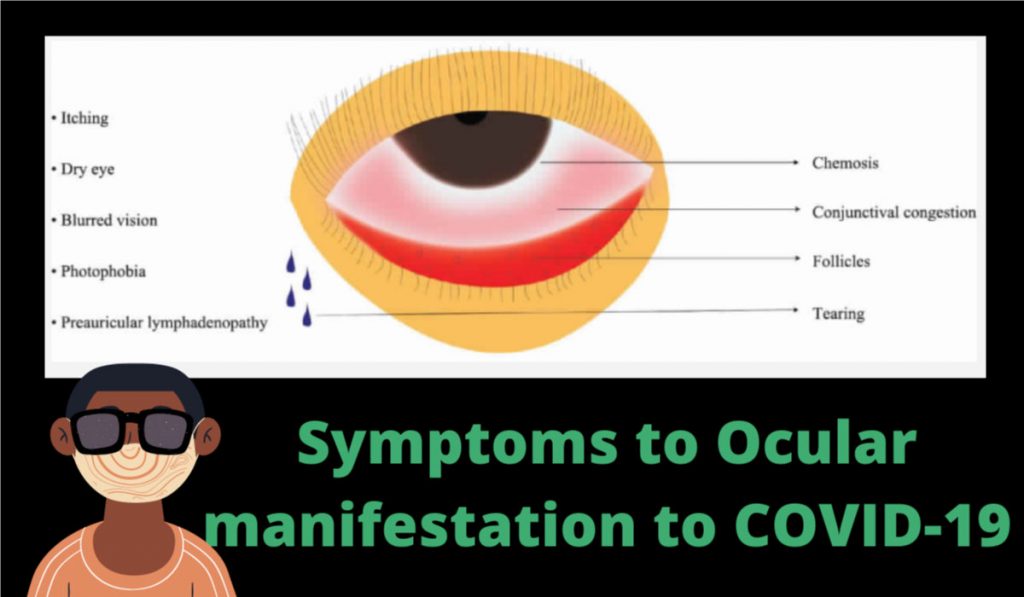
Some reports suggest that the virus can cause conjunctivitis. These reports have revealed that it can be transmitted by aerosol contact with the conjunctiva. Therefore, the suspected patient goes on the patients who are infected by a coronavirus and have travel history of domestic or international or who has visited ophthalmologist for conjunctivitis diagnosis and also have respiratory symptoms.
Conjunctivitis is an inflammation of the membrane covering the eyeball. It is often known as “pink eye.” Conjunctivitis often presents as an infected/red, “wet and weepy” eye.
Here are several studies and research that has shared their opinion about coronavirus and eye-related problems.
An eye expert at the University of Oxford, Prof Robert MacLaren, said after a recent study in Wuhan, China, where the coronavirus outbreak began, reported a range of eye problems, including swelling and sticky eye. Infected patients need to look for these symptoms too.
The New England Journal of Medicine has shared that they fond “conjunctival congestion”.
But the number of patients that are infected due with both viral conjunctivitis is known to have upper respiratory infections like cold, flu etc. and COVID-19 symptoms are very less. The approximate number found is 9 out of 1099 patients that are (0.8%).
A study in The Journal of Medical Virology found out of 30 patients hospitalized for COVID-19, only one patient diagnosed with conjunctivitis. From this information, it is very clear the occurrence of ocular manifestation to COVID-19 is very low.
Other finding included 38 patients with clinically confirmed COVID-19. Average age to these patients is around 65. Out of these, 28 patients i.e. 73.7% had positive findings for COVID-19 on RT-PCR from nasopharyngeal swabs.
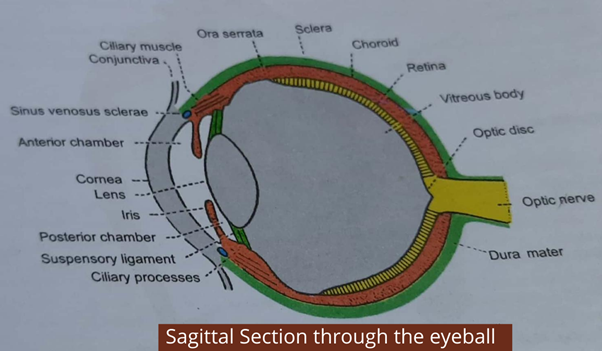
How COVID-19 does enter the human body & infects eyes?
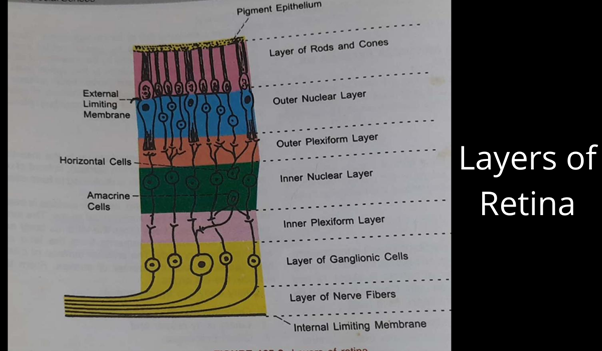
Along with Angiotensin-converting enzyme 2 (ACE2) and TMPRSS2 proteins are portals on the surface of the human cells. Coronaviruses may need heparan sulfate coreceptors, such as CD209 to enter the cells in the body. For example, on the cell surface to facilitate viral binding, especially for the highly pathogenic virus, such as SARS-CoV-2 may need help to enter the body. Check out the image shown above.
Such receptors have been detected on the eye. They are located, however, on corneal dendritic cells and conjunctival fibroblasts, which lie beneath the ocular surface and are not immediately accessible to the virus. There also are proteins in human tears, lactoferrin and 9-0-acetylated sialic acid, that can bind the virus, thereby potentially preventing its attachment to the ACE2 receptor.
Deceiving symptoms
After several observations, American Academy of Ophthalmology (AAO) passed the advice for eye care professionals to use face and eye shields while examining the patients with fever, breathlessness or any relevant or even irrelevant history of travel or even travelled to and from any hotspot that affected by the virus. There is a possibility, as conjunctivitis is the first sign to be spotted in the patient affected by COVID-19 including additional symptoms such as dry cough or anosmia.
The most important measures and outcomes to be undertaken considering ocular signs and symptoms as well as results of blood tests and RT-PCR for SARS-CoV-2. Patients who are infected and having ocular symptoms are more likely to have higher white blood cell and neutrophil counts and higher levels of procalcitonin, C-reactive protein, and lactate dehydrogenase than patients without ocular symptoms.
How to protect it?
Compared to other infections, eye issues in COVID-19 affected patients have found limited. This problem can be managed or treated with symptomatic care.
It has found at the early months when Covid had started spreading widely; it was suggested to front liners to conserve disposable medical supplies; especially by an ophthalmologist. The reason later found was only due to the shortage of medical supplies. As compared to 2003 SARS-CoV the spread of infection of SARS-COVID-19 is much higher. It has noted that health care providers are accounted for about 20% of all patients with infection.

It is, therefore, vital that proper protection of the front-line medical workers is absolutely set to be the priority.
In the absence of significant eye pain, decreased vision, or light sensitivity, many patients can be managed remotely with a trial of frequent preservative-free artificial tears, cold compresses, and lubricating ophthalmic ointment. A short course of topical antibiotics can be added to prevent or treat bacterial superinfection based on the patient's symptoms and risk factors (e.g., contact lens wear) Specific criteria are presented below.
Although preliminary studies suggest that the risk of viral transmission through ocular secretions is low, large-scale research has not yet been done, and new data is emerging daily.
Healthcare providers are, therefore, still urged to wear proper protection of the eyes, nose, and mouth when examining patients. It has been suggested that ocular transmission of the COVID-19 virus may occur.
Eye care providers and technicians may be more susceptible to infection because of the lack of distance they need to maintain while examining the patient. Eye care providers must use slit lamp breath shields. They should guide patients to speak as little as possible when sitting at the slit lamp to reduce the risk of virus transmission. The medical workers should wear a surgical mask, a face shield, and gloves. Hands are washed before and after every encounter. If a patient is positive for any of the three criteria, the full PPE of gown, face shield, gloves, and the N95 mask should be worn.
It has been noted that droplets from sneezes can travel up to 6 m. Frontline doctors and workers can use slit-lamp shield made by passing two plastic sheets through a laminator without a paper in between and cutting openings for the eye-pieces.
As a shortage of surgical masks has become a reality, some institutions are storing used masks at the end of each day in a container with a view to re-sterilization if necessary. As many as a quarter of patients being injected under sedation may develop a severe involuntary sneeze. This is more common with eyelid injections than with retrobulbar injections. Ophthalmic surgeons should be acutely aware of this to take appropriate precautions during the administration of the local anaesthetic.
The slit-lamp shields are disinfected with 70% ethyl alcohol after each patient. 70% of ethyl alcohol has been shown to reduce coronavirus infectivity. Slitlamps, b-scan probes, and any other tools are similarly cleaned with 70% ethyl alcohol. Goldman tonometers are sterilized with a 10% diluted sodium hypochlorite solution, which inactivates coronaviruses. Other disinfection and sterilization practices should be employed for shared clinic equipment such as trial frames, pinhole occluders and contact lenses for laser procedures.
Does Ocular manifestation to COVID-19 possible?
The SARS-CoV-2 infection has evolved at a tremendous rate at global health emergency in the present era. There has been a very high risk of infection that has spread like wildfire across many countries boundaries. Not only patients but also many healthcare professionals had faced the same risk. An ophthalmologist treating a non-COVID-19 infectious patient is not at risk to attract the virus. Even though the number of patients found with COVID-19 and eye issues is very less, there are very rare chances that to ocular manifestation to COVID-19. Yet, ophthalmologists must work in tandem with infectious disease specialists for risk stratification and infection control measures as well as for the use of PPE. Till the time a cure is developed, artificial intelligence-based platforms, as well as teleophthalmology, should be encouraged.
There are several myths surrounded in terms of COVID-19. Check out the table below and clear your doubts.
Myths
Facts
Nucleocapsid Protien Any Ultraviolet can kill coronavirus disease 2019 (COVID-19).
No published data is available yet on ultraviolet light affects the COVID-19 virus, its effect on other SARC virus has been studied.
Any face covering will protect against the virus.
Scarves and bandanas made of a thin fabric or a single fabric layer will not be as effective in reducing virus transmission as those that have a filter or are folded 3 to 4 times to provide a better barrier.
Wearing gloves will provide protection from the virus
Gloves will be effective if the wearer discards them after touching something that can be contaminated. After use, the gloves must be removed properly by peeling them from so they are inside out, to prevent contacting the contaminated outer surface.
All hand sanitizer are the same, and the higher the alcohol content, the better the sanitizer will work against the virus.
The alcohol content of commercially available hand sanitizer has to be at least 60% for ethyl alcohol and 70% for isopropyl alcohol to work against the virus. Alcohol content over 80% evaporated too quickly and does not stay longer on the skin to kill the virus. Hand sanitizers need to specify the type of alcohol it contains. A hand sanitizer that simply shows alcohol contains does not guarantee that it will kill the virus.
Wearing shoe covers will provide protection from virus.
If it only affective if one knows how to put them on and off very cautiously to avoid contamination. Lack of training and knowledge may cause the wearer to inadvertently touch the contaminated area.
Keywords: Coronavirus and Eye, Coronavirus & Ocular manifestation, COVID-19, Ocular infection, Does Ocular manifestation to COVID-19 possible?