Low Vision Clinic

The Low Vision Service at SRG Eye Hospital offers patients the opportunity to make the best possible use of their remaining vision through a comprehensive rehabilitative process.

The specialists use a systematic approach to the management of ocular disease that leads to permanent vision loss with a special emphasis on Age Related Macular Degeneration. The program provides a combination of special optics and re-training of the visual system for “reverse scan” reading. After the initial training is complete, patients with particular life goals are introduced to the full range of equipment to augment specific tasks like television viewing, personal accounting or personal mobility.
Low Vision
The equipment offered to patients includes:
Magnifiers
Telescopes
Optical
Electronic
Computer aids
The management of ocular disease process alone—or in combination with specialty devices—enables many patients to resume their normal activities and regain mobility and independence
Strabismus Clinic
Strabismus (say “struh-BIZ-mus”) is a vision problem in which both eyes do not look at the same point at the same time. Strabismus most often begins in early childhood. It is sometimes called crossed-eyes, walleye, or squint.
Normally, the muscles attached to each eye work together to move both eyes in the same direction at the same time. Strabismus occurs when the eye muscles don’t work properly to control eye movement. When the eye muscles don’t work as they should, the eyes may become misaligned and the brain may not be able to merge what one eye sees with what the other eye sees.
A child rarely outgrows strabismus after it has developed. Without treatment, strabismus can cause permanent vision problems. For example, if the child is not using one eye because it is misaligned, he or she can develop poor vision in that eye (called lazy eye or amblyopia).
Having strabismus can be hard on your child’s self-esteem. It affects your child’s appearance as well as his or her ability to see well. Other kids may tease your child for being cross-eyed or having a walleye. Be supportive of your child, and seek treatment right away.
What are the symptoms of strabismus?
The most common signs of strabismus are:
Eyes that don’t look in the same direction at the same time. (If your child’s eyes are only slightly misaligned, you may not notice.)
Eyes that don’t move together.
Squinting or closing one eye in bright sunlight.
Tilting or turning the head to look at an object.
Bumping into things. (Strabismus limits depth perception.)
An older child may also complain about blurred vision, tired eyes, sensitivity to light, or double vision.
Symptoms may come and go. They may get worse when your child is tired or sick.
A newborn’s eyes may be misaligned at first. But the eyes should become aligned by 3 to 4 months of age. In some cases, the eyes may simply seem to be misaligned because the child has a wide bridge of the nose that creates the appearance of crossed eyes. But if your child’s eyes aren’t aligned all of the time after age 4 months, take your child to the doctor for an eye exam.
What causes strabismus?
Childhood strabismus often has no known cause, although it tends to run in families. Sometimes strabismus develops when the eyes compensate for other vision problems, such as farsightedness or a cataract. Other things that can increase your child’s risk for strabismus include an illness that affects the muscles and nerves, premature birth, Down syndrome, a head injury, and other problems. Adults may develop strabismus from eye or blood vessel damage. Loss of vision, an eye tumor or a brain tumor, Graves’ disease, stroke, and various muscle and nerve disorders can also cause strabismus in adults.
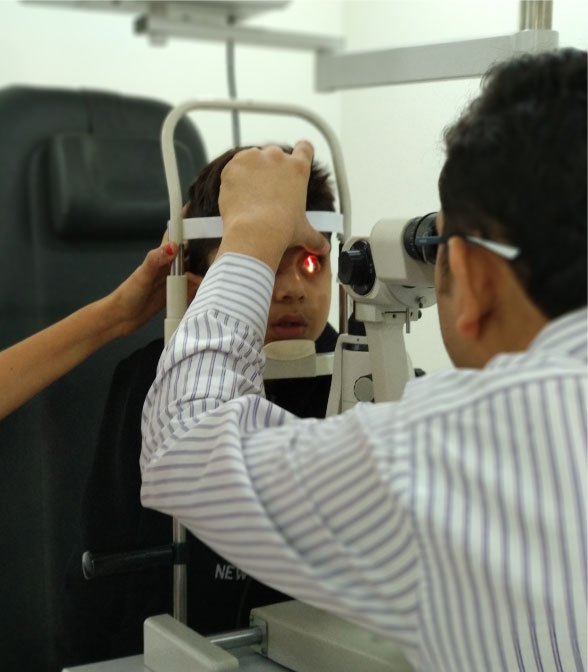
How is strabismus diagnosed?
A doctor can often tell that a child has strabismus just by looking at the child’s eyes. It may be obvious that the eyes don’t look in the same direction at the same time. The doctor may have the child look at an object while covering and then uncovering each eye. This allows the doctor to see which eye turns, how much it turns, and under what circumstances the abnormal turn occurs. These tests will also help the doctor find out if the child has amblyopia (lazy eye), which sometimes occurs with strabismus. Most experts suggest that children have an eye exam between the ages of 3 and 5, and earlier in some cases. But no child is too young for an eye exam. If you have concerns about your child’s eyes or vision at any age, take him or her to an eye doctor.
How is strabismus treated?
The most common treatments for strabismus are:
Glasses. Wearing glasses can sometimes correct mild strabismus.
A temporary eye patch over the stronger eye if your child has amblyopia. This can make the weak eye stronger, which may help align the eyes. Your child may have to wear the patch some or all of the time for a few weeks or months.
Surgery on the eye muscles. This is often the only way to improve vision and better align the eyes. It may take more than one surgery, and your child may still need to wear glasses.
Other treatments may include medicines and eye exercises. Treatment for strabismus should begin as soon as possible. In general, the younger the child is when treatment begins, the better the chances are of correcting the problem. It’s also important for your child to get follow-up exams.
What are the symptoms of strabismus?
The most common signs of strabismus are:
What causes strabismus?
Childhood strabismus often has no known cause, although it tends to run in families. Sometimes strabismus develops when the eyes compensate for other vision problems, such as farsightedness or a cataract. Other things that can increase your child’s risk for strabismus include an illness that affects the muscles and nerves, premature birth, Down syndrome, a head injury, and other problems. Adults may develop strabismus from eye or blood vessel damage. Loss of vision, an eye tumor or a brain tumor, Graves’ disease, stroke, and various muscle and nerve disorders can also cause strabismus in adults.
How is strabismus diagnosed?
A doctor can often tell that a child has strabismus just by looking at the child’s eyes. It may be obvious that the eyes don’t look in the same direction at the same time. The doctor may have the child look at an object while covering and then uncovering each eye. This allows the doctor to see which eye turns, how much it turns, and under what circumstances the abnormal turn occurs. These tests will also help the doctor find out if the child has amblyopia (lazy eye), which sometimes occurs with strabismus. Most experts suggest that children have an eye exam between the ages of 3 and 5, and earlier in some cases. But no child is too young for an eye exam. If you have concerns about your child’s eyes or vision at any age, take him or her to an eye doctor.
How is strabismus treated?
The most common treatments for strabismus are:
Other treatments may include medicines and eye exercises. Treatment for strabismus should begin as soon as possible. In general, the younger the child is when treatment begins, the better the chances are of correcting the problem. It’s also important for your child to get follow-up exams.
Diabetic Retinopathy
The disease takes two forms:
Early diabetic retinopathy
Advanced diabetic retinopathy
The longer you have diabetes and the less you regulate your blood sugar, the more likely you are to develop this condition. If you have diabetes, see an ophthalmologist for a full eye exam yearly. Finding and treating problems early may save your sight. If your vision changes suddenly or becomes blurry, spotty or hazy, schedule an exam by one of our ophthalmologists right away.
What are the Symptoms of Diabetic Retinopathy?
At first, you may not have symptoms or they may be mild. As the disease progresses, you may experience:
Spots or dark strings floating in your vision (floaters)
Blurred vision
Fluctuating vision
Impaired color vision
Dark or empty areas in your vision
Vision loss
Protecting yourself against diabetes is the best way to avoid retinopathy. If you are already diabetic, regular eye exams, controlling your blood sugar, and blood pressure are essential to preventing this disease. Diabetics need vision experts on their health care team. At Bascom Palmer Eye Institute, part of the University of Miami Health System, our skilled retinal specialists partner with you to protect your vision.
Diabetic Retinopathy: Tests
Comprehensive Eye Exam – During your exam, your eye care professional dilates your eyes and evaluates your vision for several factors. If necessary, additional tests/procedures may be used to confirm your diagnosis.
Fluorescein Angiography – This test helps your doctor see changes in the structure or function of your retinal blood vessels. To perform this test, your doctor injects a fluorescent yellow dye into a vein in your arm or hand, then photographs your retina as the dye outlines your blood vessels.
Indocyanine Green Angiography (ICG) – This test uses an injectable dye and special cameras to find blood circulation issues in the choroid. The choroid is a layer of blood vessels under the retina.
Optical Coherence Tomography (OCT) – This imaging technique provides cross-sectional views of your retina. This helps your physician see if there is any abnormal swelling in your retina.
Ultrasound Imaging – This safe, painless test uses high-frequency sound waves to produce detailed images of the inside of your eye. This helps your doctor identify retinal damage.
Diabetic Retinopathy: Treatments
Focal Laser Treatment – Also known as photocoagulation, focal laser treatment stops or slows blood flow from leaking inside the eye.
Scatter Laser Treatment – This treatment, also called panretinal photocoagulation, uses a laser to destroy damaged retina, to prevent the formation of abnormal blood vessels and scar tissue that could lead to vision loss. Laser surgeries work best if your condition is not advanced. These laser treatments are outpatient procedures and do not require general anesthesia.
Pharmacologic Therapies – Medications used directly in the eye have shown promise in treating some forms of the disease.
Vitrectomy – If your condition is severe, your surgeon may perform a vitrectomy. To perform this treatment, the surgeon makes small incisions in your eye, removes any abnormal blood or scar tissue and may administer laser treatment or medictine into the eye.
The longer you have diabetes and the less you regulate your blood sugar, the more likely you are to develop this condition. If you have diabetes, see an ophthalmologist for a full eye exam yearly. Finding and treating problems early may save your sight. If your vision changes suddenly or becomes blurry, spotty or hazy, schedule an exam by one of our ophthalmologists right away.
What are the Symptoms of Diabetic Retinopathy?
At first, you may not have symptoms or they may be mild. As the disease progresses, you may experience:
Protecting yourself against diabetes is the best way to avoid retinopathy. If you are already diabetic, regular eye exams, controlling your blood sugar, and blood pressure are essential to preventing this disease. Diabetics need vision experts on their health care team. At Bascom Palmer Eye Institute, part of the University of Miami Health System, our skilled retinal specialists partner with you to protect your vision.
Diabetic Retinopathy: Tests
Comprehensive Eye Exam – During your exam, your eye care professional dilates your eyes and evaluates your vision for several factors. If necessary, additional tests/procedures may be used to confirm your diagnosis.
Fluorescein Angiography – This test helps your doctor see changes in the structure or function of your retinal blood vessels. To perform this test, your doctor injects a fluorescent yellow dye into a vein in your arm or hand, then photographs your retina as the dye outlines your blood vessels.
Indocyanine Green Angiography (ICG) – This test uses an injectable dye and special cameras to find blood circulation issues in the choroid. The choroid is a layer of blood vessels under the retina.
Optical Coherence Tomography (OCT) – This imaging technique provides cross-sectional views of your retina. This helps your physician see if there is any abnormal swelling in your retina.
Ultrasound Imaging – This safe, painless test uses high-frequency sound waves to produce detailed images of the inside of your eye. This helps your doctor identify retinal damage.
Diabetic Retinopathy: Treatments
Focal Laser Treatment – Also known as photocoagulation, focal laser treatment stops or slows blood flow from leaking inside the eye.
Scatter Laser Treatment – This treatment, also called panretinal photocoagulation, uses a laser to destroy damaged retina, to prevent the formation of abnormal blood vessels and scar tissue that could lead to vision loss. Laser surgeries work best if your condition is not advanced. These laser treatments are outpatient procedures and do not require general anesthesia.
Pharmacologic Therapies – Medications used directly in the eye have shown promise in treating some forms of the disease.
Vitrectomy – If your condition is severe, your surgeon may perform a vitrectomy. To perform this treatment, the surgeon makes small incisions in your eye, removes any abnormal blood or scar tissue and may administer laser treatment or medictine into the eye.
Uveitis
Uveitis is a general term for inflammation and infections inside the eye. Depending on which part of your eye is affected, you may be diagnosed with something more specific. For example, when the pigmented parts of your eye including the colored iris, are inflamed, it is called iritis or anterior uveitis. Other types of uveitis are vitritis (intermediate uveitis) and retinitis or choroiditis (posterior uveitis). No matter where the inflammation is located or what caused it, this condition can affect vision and cause complications in other vital parts of your eye.
Because uveitis occurs for many reasons, seeing a qualified eye specialist is important. The skilled physicians at Bascom Palmer Eye Institute, part of the University of Miami Health System, examine your eyes thoroughly to ensure that you get the right treatment for your specific situation. If an eye injury or infection caused your uveitis, your treatment focuses on that particular condition. If a disease elsewhere in your body caused the uveitis, you may be able to control it by treating the underlying cause.
What Are the Symptoms of Uveitis?
Typically, symptoms appear suddenly and worsen quickly. They may include:
Eye redness
Eye pain
Light sensitivity
Blurred vision
Dark, floating spots in your field of vision (floaters)
Decreased vision
What Causes Uveitis?
Many conditions cause uveitis, including:
Eye injury or surgery
Inflammations related to the eye, such as birdshot chorioretinopathy or pars planitis
Inflammations related to other disorders, such as sarcoidosis, ankylosing spondylitis, juvenile idiopathic arthritis or Crohn’s disease
Infections inside or outside the eye, such as cat-scratch disease, herpes zoster, syphilis, toxoplasmosis, tuberculosis, Lyme disease or West Nile virus
Cancers that affect the eye, such as lymphoma
Recent studies also show uveitis is more common and more severe in people who smoke cigarettes. If you have uveitis and smoke cigarettes, you should consider stopping. Eye inflammation may lead to more serious problems if left untreated, including other eye diseases such as glaucoma, cataracts or loss of eyesight. If you have been diagnosed with uveitis or a related condition called scleritis, schedule an exam with one of our specialty ophthalmologists.
Uveitis: Tests
Blood Tests and X-rays – Certain standard blood tests are performed on all uveitis patients. If necessary, more testing focused specifically on your condition, including X-Rays, will be done. You may need to see a medical specialist to help with your diagnosis.
Eye Fluid Analysis – In some cases, your doctor may take a small sample of fluid from the front part of your eye to help diagnose your condition rather than perform a vitrectomy. Some viral infections can be diagnosed in this way.
Eye Angiography – Photographs of the eye, taken after fluorescent dyes are injected into a vein in your arm, help evaluate blood flow in the retinal blood vessels. This helps your doctor determine if the retina or uvea in the back of the eye is inflamed.
Eye Photography – Using the most modern photographic techniques, your doctor examines the inside of your eye, measuring the thickness of the retina and detecting other signs of inflammation. These tests take only seconds to perform and are easy and painless for patients.
Uveitis: Treatments
Oral Medications – Many medications treat uveitis, but treatment must be tailored to your specific condition.
Injected Medications – When injected into the eye, drugs such as corticosteroids, slow-dissolving steroid pellets or very slow steroid release devices help some patients control their uveitis.
Vitrectomy – Removing the vitreous (a gel-like substance in the middle of your eye) may help control uveitis if you have intermediate uveitis. Vitrectomy is also used to remove vitreous samples for study in the lab to reach a more precise diagnosis.
Because uveitis occurs for many reasons, seeing a qualified eye specialist is important. The skilled physicians at Bascom Palmer Eye Institute, part of the University of Miami Health System, examine your eyes thoroughly to ensure that you get the right treatment for your specific situation. If an eye injury or infection caused your uveitis, your treatment focuses on that particular condition. If a disease elsewhere in your body caused the uveitis, you may be able to control it by treating the underlying cause.
What Are the Symptoms of Uveitis?
Typically, symptoms appear suddenly and worsen quickly. They may include:
What Causes Uveitis?
Many conditions cause uveitis, including:
Recent studies also show uveitis is more common and more severe in people who smoke cigarettes. If you have uveitis and smoke cigarettes, you should consider stopping. Eye inflammation may lead to more serious problems if left untreated, including other eye diseases such as glaucoma, cataracts or loss of eyesight. If you have been diagnosed with uveitis or a related condition called scleritis, schedule an exam with one of our specialty ophthalmologists.
Uveitis: Tests
Blood Tests and X-rays – Certain standard blood tests are performed on all uveitis patients. If necessary, more testing focused specifically on your condition, including X-Rays, will be done. You may need to see a medical specialist to help with your diagnosis.
Eye Fluid Analysis – In some cases, your doctor may take a small sample of fluid from the front part of your eye to help diagnose your condition rather than perform a vitrectomy. Some viral infections can be diagnosed in this way.
Eye Angiography – Photographs of the eye, taken after fluorescent dyes are injected into a vein in your arm, help evaluate blood flow in the retinal blood vessels. This helps your doctor determine if the retina or uvea in the back of the eye is inflamed.
Eye Photography – Using the most modern photographic techniques, your doctor examines the inside of your eye, measuring the thickness of the retina and detecting other signs of inflammation. These tests take only seconds to perform and are easy and painless for patients.
Uveitis: Treatments
Oral Medications – Many medications treat uveitis, but treatment must be tailored to your specific condition.
Injected Medications – When injected into the eye, drugs such as corticosteroids, slow-dissolving steroid pellets or very slow steroid release devices help some patients control their uveitis.
Vitrectomy – Removing the vitreous (a gel-like substance in the middle of your eye) may help control uveitis if you have intermediate uveitis. Vitrectomy is also used to remove vitreous samples for study in the lab to reach a more precise diagnosis.
ARMD
The macula is a specialized portion of the retina responsible for central vision. Located at the back of your eye in the center of your retina, the macula provides the sharp vision you need to drive, to read and to see details. However, if you’re over the age of 50, age-related macular degeneration (AMD) may affect your ability to see. In fact, among older people, AMD is the main reason for irreversible legal blindness . The disease runs in families and is much more severe in people who smoke.
There are two types of AMD:
Dry AMD is the first stage of the disease. It starts slowly, eventually leading to loss of central vision. While the disease affects both eyes and progresses faster in one eye compared to the other, most people eventually lose their central vision in both eyes.
Wet AMD arises from Dry AMD and is characterized by the growth of abnormal blood vessels in your macula. These abnormal blood vessels leak fluid and blood. If untreated, then this fluid and blood causes a scar to form and significant vision loss occurs. If the Wet AMD is treated, then it can be converted back to Dry AMD.
When Should You See a Doctor?
Dry AMD progresses slowly, but the use of vitamin supplementation and a diet rich in dark-green leafy vegetables can help slow down the vision loss if you catch the problem early. That’s why regular eye exams matter. If you can’t see people clearly at a distance, have trouble transitioning from dark to bright light, or if you need increasingly brighter light to read by, schedule an appointment with an eye doctor. Wet AMD damages the macula much more quickly. Again, if you experience noticeable differences in your sight, especially blurry or distorted vision, then consult an eye doctor as soon as possible. AMD is worrisome for older people, but with proper diagnosis, the experts at Bascom Palmer Eye Institute, part of the University of Miami Health System, will help you manage your condition and protect your vision.
ARMD: Tests
Comprehensive Eye Exam – The standard way of diagnosing macular degeneration is with a dilated exam. During your examination, your ophthalmologist will search for retinal damage and may perform other tests.
Distance Visual Acuity Measurement – In this test, you cover one eye, read a standard eye chart from a distance and then repeat the process with the other eye. Your eye care professional records how well your eyes see at a distance.
Amsler Grid – In this test, you look at an Amsler grid’s pattern of straight horizontal and vertical lines. If you have AMD, you will see wavy lines, distorted or missing lines or a black spot in the center of the grid.
Optical Coherence Tomography (OCT) – This non-invasive imaging procedure uses dim light and produces a cross-sectional, three-dimensional (3-D) images of the inside of your eyes. By performing OCT imaging, you doctor can determine if your AMD is getting worse and whether you need an injection into your eye.
Fluorescein Angiography – Using this method, your doctor can see changes in the structure or function of your retinal blood vessels. To perform the test, your eye care professional injects dye into a vein in your arm or hand, then photographs your retina as the dye outlines your blood vessels. Click here to watch a video about macular degeneration
ARMD: Dry AMD Treatment
AREDS2 Vitamin, Multivitamin, and Dark Green Leafy Vegetables – Research shows that high-levels of certain vitamins and zinc reduce the risk of Wet AMD by up to 25 percent. These over-the-counter vitamins are currently the only treatment for Dry AMD. In addition, a daily serving of cooked or raw dark-green leafy vegetables is recommended. If you are a smoker, then stop immediately.
ARMD: Wet AMD Treatments
Anti-VEGF Injections – Injections of drugs into the eye that block vascular endothelial growth factor (anti-VEGF injections) prevent the severe vision loss that normally occurs in WET AMD, and in many patients, vision is improved. If your doctor recommends this treatment, then the injections need to be given every month at first, and then the injections can be spaced out and become less frequent. By stopping or limiting the growth of new blood vessels, this medication helps preserve your vision.
There are two types of AMD:
When Should You See a Doctor?
Dry AMD progresses slowly, but the use of vitamin supplementation and a diet rich in dark-green leafy vegetables can help slow down the vision loss if you catch the problem early. That’s why regular eye exams matter. If you can’t see people clearly at a distance, have trouble transitioning from dark to bright light, or if you need increasingly brighter light to read by, schedule an appointment with an eye doctor. Wet AMD damages the macula much more quickly. Again, if you experience noticeable differences in your sight, especially blurry or distorted vision, then consult an eye doctor as soon as possible. AMD is worrisome for older people, but with proper diagnosis, the experts at Bascom Palmer Eye Institute, part of the University of Miami Health System, will help you manage your condition and protect your vision.
ARMD: Tests
Comprehensive Eye Exam – The standard way of diagnosing macular degeneration is with a dilated exam. During your examination, your ophthalmologist will search for retinal damage and may perform other tests.
Distance Visual Acuity Measurement – In this test, you cover one eye, read a standard eye chart from a distance and then repeat the process with the other eye. Your eye care professional records how well your eyes see at a distance.
Amsler Grid – In this test, you look at an Amsler grid’s pattern of straight horizontal and vertical lines. If you have AMD, you will see wavy lines, distorted or missing lines or a black spot in the center of the grid.
Optical Coherence Tomography (OCT) – This non-invasive imaging procedure uses dim light and produces a cross-sectional, three-dimensional (3-D) images of the inside of your eyes. By performing OCT imaging, you doctor can determine if your AMD is getting worse and whether you need an injection into your eye.
Fluorescein Angiography – Using this method, your doctor can see changes in the structure or function of your retinal blood vessels. To perform the test, your eye care professional injects dye into a vein in your arm or hand, then photographs your retina as the dye outlines your blood vessels. Click here to watch a video about macular degeneration
ARMD: Dry AMD Treatment
AREDS2 Vitamin, Multivitamin, and Dark Green Leafy Vegetables – Research shows that high-levels of certain vitamins and zinc reduce the risk of Wet AMD by up to 25 percent. These over-the-counter vitamins are currently the only treatment for Dry AMD. In addition, a daily serving of cooked or raw dark-green leafy vegetables is recommended. If you are a smoker, then stop immediately.
ARMD: Wet AMD Treatments
Anti-VEGF Injections – Injections of drugs into the eye that block vascular endothelial growth factor (anti-VEGF injections) prevent the severe vision loss that normally occurs in WET AMD, and in many patients, vision is improved. If your doctor recommends this treatment, then the injections need to be given every month at first, and then the injections can be spaced out and become less frequent. By stopping or limiting the growth of new blood vessels, this medication helps preserve your vision.
Aesthetics
People pursue cosmetic surgical and non-surgical treatments for many reasons. Some men and women wish to reduce the signs of aging. Adults and children with birth defects, eyelid disorders or injuries may need reconstructive surgery to improve their vision and appearance. When they receive expert treatment, these patients benefit from improved well-being, self-image, and in many cases, better vision.
Our Doctors have the skill and experience needed to perform delicate eyelid and facial procedures. Facial surgery or non-surgical cosmetic treatments that may affect your vision.
