Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
Retinal Detachment: Causes, Symptoms, Diagnosis and Treatment
What is Retina?
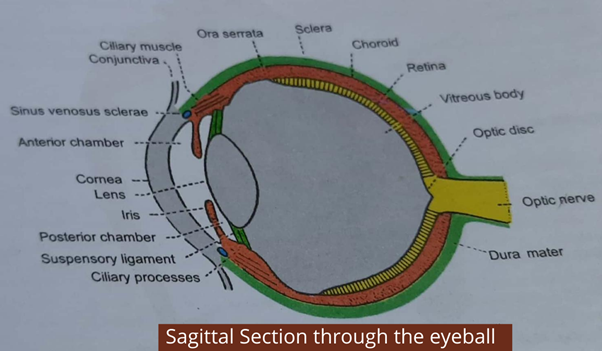
Retina or the inner coat of the eye is the thin, delicate inner layer of the eyeball. The retina is continuously the hindered part of the body with the optic nerve. The retina lacks in thickness from behind and forward.
The optic part of the retina contains nervous tissues and is sensitive to light. The depressed area of the optic disc is called the physiological cup. It contains no rods or cones and is therefore insensitive to light. The rods and cones are light receptors of the eye. The rods contain a pigment called visual purple. Rods can respond to dim light (scotopic vision). Cones respond only to bright light (photopic vision) and are sensitive to colour.
What is Retinal Detachment?
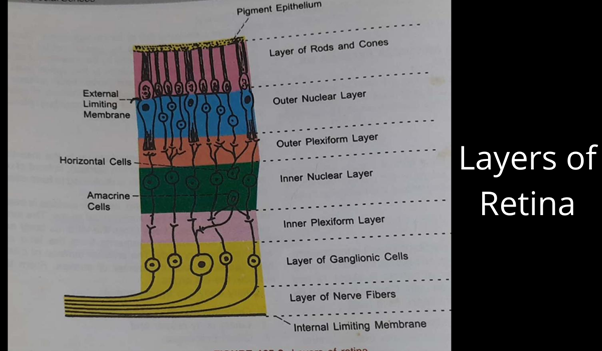
- The outer pigmented layer
- The layer of rods and cones
- External limiting membrane
- Outer nuclear layer
- Outer plexiform layer
- Inner nuclear layer (bipolar cells)
- Inner plexiform layer
- Ganglion cell layer
- Nerve fibre layer
- The internal limiting membrane
So when the detachment of the retina takes place, the outer pigmented layer remains attached to the choroid, but all the remaining nine layers of the retina separate from the pigmented layers and are displaced inwards which ultimately affects the retina.
What are the symptoms of Retinal Detachment?
After the retina is detached from the back wall of the eye that is from sclera and dura mater and the eye no longer functions properly. It creates several problems for the visuals.Initial symptoms are very mere like flashing light (photopsias) and floaters (floating spots in the vision). These are also the symptoms of retinal tear or separation of the vitreous gel from the retina. So when someone is facing the symptom of flashing lights that means the vitreous gel is pulling on and covering the retina. This occurs due to the looseness of the vitreous gel it bumps on the retina. This usually occurs when the person is aged and egg-like gel becomes runny.
When the patients complain about flashing lights, they actually mean brief lighting streaks are seen in the outer layer of the eyes. These flashes may cause due to pressure or force on the retina. The floaters are usually described by the patients as strands, spots or little flies. Sometimes patients may also experience a shadow or curtain that prevent them from clear vision. When any of these symptoms are described by the patients there is mostly the chances that the central macular area of the retina detached from the outer pigmented layer.
What are the causes of Retinal Detachment?

There are several reasons which can cause a detached retina. But the three major reasons are:
Rhegmatogenous is a tear in the retina. A tear can be caused by the age when vitreous fluid starts getting thinner and free from its original place.
Vitreous body fluid is generally being thick more like jelly-white consistency and when it starts separating from retina causes a tear in the retina. The vitreous body fills the posterior segment of the eyeball.From the behind it is attached to the optic disc, and in front to the ora Serrata; in between it is free and lies in contact with the retina.
There is certainly a chance in the patient for a rhegmatogenous detached retina, especially if the patient has gone through cataract surgery, the age of the patient is more, if the case of myopia is too high, or has had a family history of a detached retina, or if the outer edges or the layers of the retina has thinned which is known as lattice degeneration.
When vitreous fluid overlaps on the retina and enters choroid and retina. This process of overlapping of fluid makes retina tent up away from the choroid. This is a very less common type of detached retinal which is known as tractional detachment. Usually, tractional detachment occurs when the patient has a diabetic eye disease. Diabetic eye disease is a disease in which vitreous body fluid draws on to abnormal blood vessels that are on the retina.
The third and rarest condition of retinal detachment occurs only due to dreadful circumstances. Such circumstances include any inflammatory situations near-eye which will lead fluid to leaks out of the blood vessel causing damaged and collecting underneath the retina. This process will certainly create a curtain which will prevent the patient from a clear vision. Such conditions are known uveitis and scleritis or tumours of the eyes or even autoimmune disease, and also congenital disease may occur in such situation like Coat’s disease.
Who is at Risk for Retinal Detachment?
Aforementioned are the causes, it is quite clear by now that which are those factors that may cause growth in the risk of developing the detached retina.
- Family history. In case, any family member has had faced or had the history of retinal detachment then it is likely that someone in the family may catch the symptoms sooner or later.
- Usually, the case of the detached retina is found in the middle or at an old age patient. But in very rare cases children may show these symptoms which is majorly the type of tractional detached retina known as retinopathy of prematurity. This condition is seen in premature infants who receive oxygen in the high-risk neonatal nursery.
- Someone has the extreme nearsightedness (myopia) is likely to prone retinal detachment.If any patient has already undergone the retinal detachment surgery is also prone to the symptoms again in the future but not in every case.
- If some patient has undergone through any complicated cataract-removal surgery should be aware of the possibility of a detached retina.
- In case someone has been into any sort of trauma that is closer or directly related to the eye may cause damage to the blood vessel in the eye which will ultimately lead to the gathering of blood near retina which will eventually cause uveitis and scleritis or tumours of the eyes or even autoimmune disease, and also congenital disease.
Which are the possible ways to diagnose retinal detachment?
The diagnosis of retinal detachment is usually treated by Ophthalmologists. Ophthalmologist doctor is capable of treating any eye problems including vision. After 12 to 13 years to education and practise, some doctors are further trained to in specific medical or surgical eye care. These subspecialist doctors have to undergo through one or two years of the comprehensive studies training programme which is also known as Fellowship. After training, these subspecialist doctors are capable to treat diseases like Glaucoma, Retinal detachment, any other problems related to retina, Cornea, Pediatrics, Neurology, Ocular-Plastic Surgery and also vitreoretinal surgery.
Ophthalmologist’s doctors may use three different types of diagnosis ways for retinal detachment:
Through Instruments:
Doctors may use a special instrument which releases a bright light that will examine the back of your eye. It can also be done by using a special kind of lenses. These both ways can identify if your retina has any sort of tear or holes or detachment from the choroid.
Ultrasound image testing:
This method of diagnosis is done for the patients whose blood vessel are damaged and the bleeding had occurred. Bleeding in the eye makes it difficult for your doctor to see even through special lenses. However, ultrasound image testing helps the doctor to have a clear vision of your eye.
To diagnose retinal detachment, your doctor will perform a thorough eye exam. They’ll check:
- For the clear vision of the eye
- Any kind of pressure in the eye
- The physical appearance of the eye
- Ability to see colours
What are the possible ways to treat retinal detachment?
If you are diagnosed with any issue with your retina, maybe a hole or a tear or if your eye is bleeding, you are at high risk of developing retinal detachment. The reason why it is better in case if you are having any of the symptoms mentioned above.
There is two basic procedure of the retinal detachment:
Laser Photocoagulation:
Laser Photocoagulation treatment is mostly done when the retina is found with a tear on it. This procedure is relatively painless and largely practised. During the procedure, your doctor will first numb your eye with anaesthetic eye drops. After a few minutes, the bright light laser is focused through your eye which creates the scar or burns the area beside the retinal tear or any small detachment. The scar tissue will naturally help the tear or the detached retina to reattached that particular portion.
Cryotherapy:
Another way to treat a tear or a hole or retinal detachment is by Cryotherapy. Cryotherapy procedure is done by inserting a freezing probe in your eye. The probe is inserted next to affected tissue or nerve or the tear. The freezing probe inactivates the nerve. Every time the area is frozen by the probe; the scar tissue is formed. Then on the scar tissue helps the tear or the detached retina to fill attach is its natural way.
This procedure may take a little more time than laser photocoagulation as eye surgeon has to use the freezing probe several times to make the scar.
There are further three different procedures that are based on the location, size of the retinal detachment or if the patient has had any cataract surgery earlier.
Pneumatic Retinopexy:
For this procedure, your eye surgeon will first numb your eye. After doctor will inject intraocular gas bubble in a vitreous portion of your eye to help your retina move back into place up against the wall of your eye. Once your retina is back in place, your doctor will use a laser photocoagulation treatment or freezing probe (Cryotherapy treatment) to seal the holes.
Scleral buckling:
For severe detachments or delicate location of the detachment, the patient will need to have eye surgery in a hospital. Your doctor may recommend scleral buckling procedure to push retina at the back of your eye. This involves placing a small silicone band around the outside of your eye that is at sclera. To keep the band at its place, the eye surgeon will have to sew the silicon band. This buckle stays in your eye permanently. Scleral buckling may be done in combination with a vitrectomy. Cryopexy or retinopexy is performed during the scleral buckle procedure.
Vitrectomy:
Another option is vitrectomy, which is used for larger tears. This procedure involves anaesthesia and is often performed as an outpatient procedure, but may require an overnight stay in the hospital. Your doctor will use small tools to enter through the sclera of the eye and inserts an instrument that will remove vitreous, a gel-like fluid from your retina. Then the surgeon will place your retina back into its proper place by following laser photocoagulation or cryotherapy. To place retina at its original place, the doctor will again inject intraocular gas and replace the vitreous gel. This procedure will automatically push retina at its original place.
What to expect after retinal surgery?
The positioning of your head- Most of the time, your eye surgeon will ask you to keep your head at a certain position for a few days or weeks after the surgery. This way it will be safe that gas bubble or band will not leave its original place and it will help the retina to reattach.
Avoid flying in an aeroplane.
Avoid having nitrous oxide for anaesthesia or the intraocular gas may expand and may cause lasting damage to your eye.
Topical steroids or antibiotics are suggested by the doctor after the surgery so as to avoid any risk of bleeding or inflammation or any other complications after the surgery.
After the surgery, it may take several weeks or a month to have a complete and clear vision. However, it may happen with certain patients that they may have to undergo through cataract surgery after retinal detachment surgery as the retinal surgery may trigger changes in the lens of the eye. After the retinal surgery, the doctor may ask the patient to avoid heavy lifting or exercises, or bending down for first few weeks.


